GPs should proactively check if their enrolled patients have completed their ACP. If they have not done so, GPs should encourage them to complete their ACP during the annual health plan check-in. GPs can use the ACP collaterals (please see Additional Resources section below) to advocate about ACP. AIC is developing an online training resource to support GPs in becoming a stronger advocate for ACP to their patients – this will be available by Oct 2025.
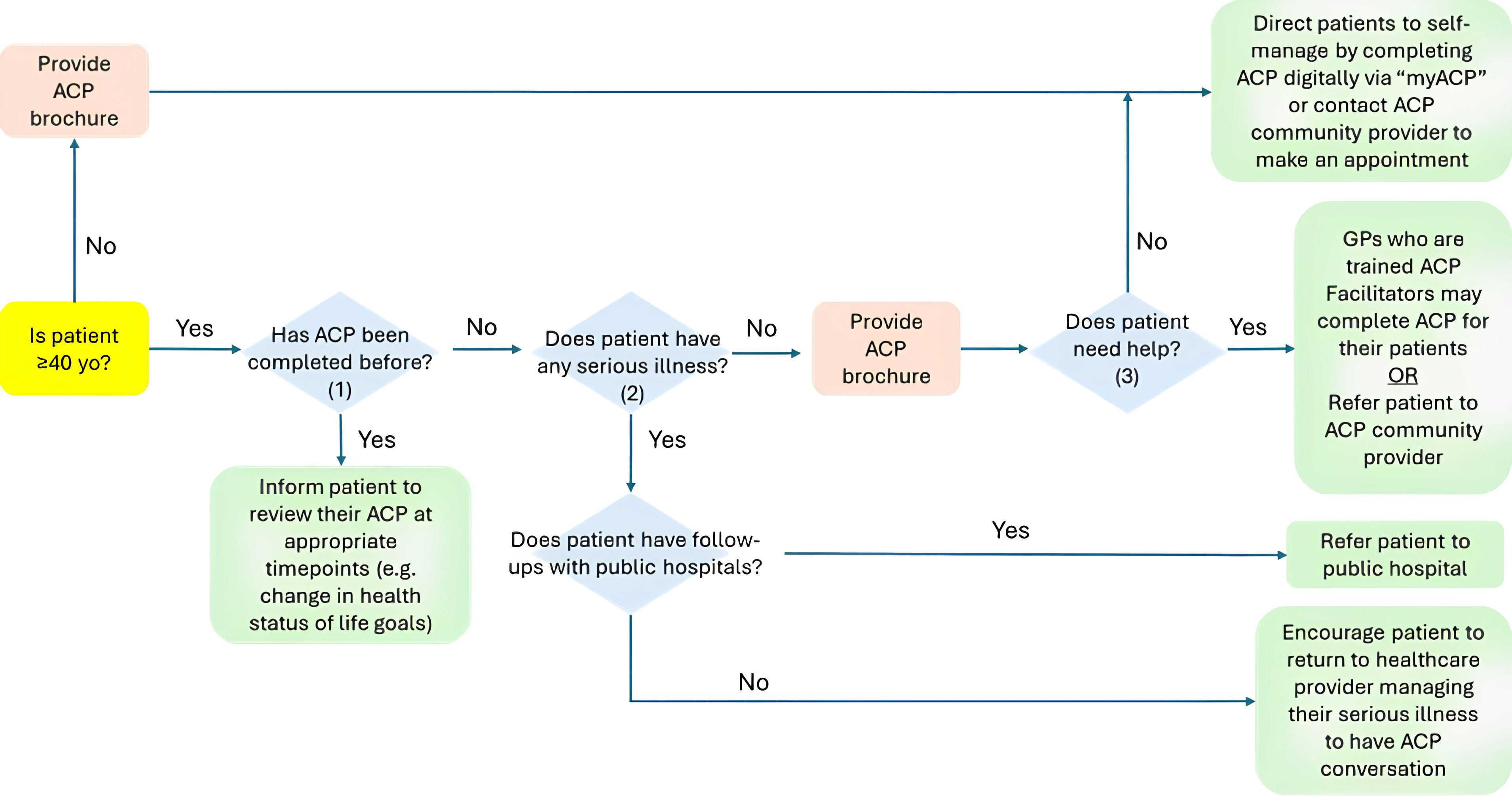
GPs who are trained as ACP facilitators may complete ACP with their patients. GPs may also signpost or refer patients to (Figure 1: Referral Pathway):
(i) myACP on the My Legacy portal, for well patients in general, with no serious illness(es)*
Patients can complete their ACP online through myACP. This is free of charge. ACP self-documentation can be considered for most patients. They or their relevant NHS should be familiar with navigating governmental e-services.
(ii) ACP community providers, for patients with no serious illness(es)* but need face-to-face assistance
GPs may refer to Find an ACP Service Provider for ACP community providers' referral contacts. GPs should direct their patients to either book their appointments directly from the site or to call the ACP community provider directly using the listed phone number to make the ACP appointment.
(iii) their respective public hospital, for patients who have serious illness(es)*
GPs may refer to Find an ACP Service Provider for public hospitals' referral contacts. GPs should direct their patients to call the public hospital via the listed phone number to make the ACP appointment. From April 2026, GPs may make referrals for their patients to public hospitals using their Healthier SG-compatible CMSes.
*Serious illness(es) include, but are not limited to: Cancer, Chronic Neurological Diseases, Chronic Obstructive Pulmonary Disease (COPD) and End-Stage Lung Disease, Dementia, End-Stage Renal Failure (ESRF), Heart Failure, Severe Liver Disease.
GPs should also encourage all enrollees to review their ACP at appropriate timepoints (e.g. when there are changes in their health statuses, activities of daily living and life goals).
Figure 1: Referral Pathway
Notes
(1) Patients can check on MyLegacy; GPs may also refer to National Electronic Health Records (NEHR)
(2) Serious illness(es) include, but are not limited to: Cancer, Chronic Neurological Diseases, Chronic Obstructive Pulmonary Disease (COPD) and End-Stage Lung Disease, Dementia, End-Stage Renal Failure (ESRF), Heart Failure, Severe Liver Disease
(3) Factors to consider include: (a) presence of serious illnesses, (b) possession of SingPass and ability to use governmental e-services, (c) has an NHS with a SingPass account, (d) patient's understanding of their health and disease trajectory

